
The Black/African American Healthcare Experience: Where Disparities Persist and Why It Matters
Filed Under: Market Research, Black / African American, Multicultural, CPG, Health Insurance
Ashleigh Williams
Senior Director, In-Person Qualitative Research

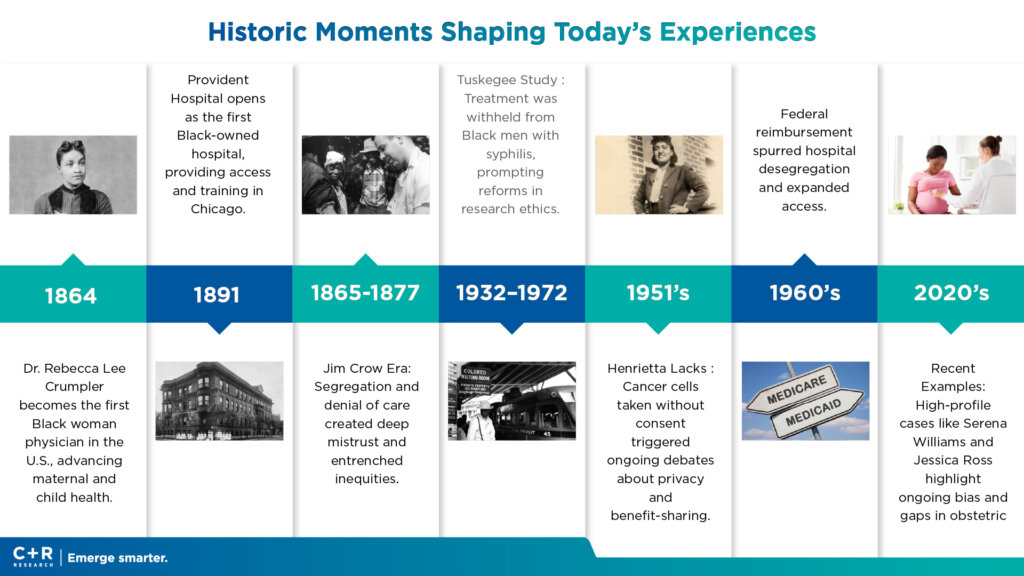
This month, we’re partnering across C+R’s Multicultural and Healthcare specialties to spotlight an issue drawing intensified national attention: healthcare experiences in the Black/African American community. From rising premiums and coverage churn to widely shared patient stories—like recent incidents where Black mothers in active labor were delayed or turned away, resulting in dangerous births outside of proper care like Mercedes Wells and Kiara Jones—these are not isolated events or “new” phenomena. They’re the latest chapters in a long, intergenerational history of mistrust, unequal treatment, and structural barriers that continue to shape how Black/AA consumers engage with the U.S. health system today.
These stories circulate in families—from grandmother to mother to daughter—and inform behaviors: how appointments are scheduled (or avoided), where care is sought (or substituted), and which products are chosen to manage health and wellness at home. To kick this story off we want to ground you in this journey of understanding with some overarching insights and statistics that give you a detailed picture of what Black/African Americans experience daily as they navigate healthcare spaces.

The Evidence: Where Disparities Show Up—and Why They Persist
1) Access to Coverage and Care
Black Americans remain more likely to be uninsured, and more likely to delay or forgo care due to cost. In 2023, 9.7% of Black people under 65 were uninsured vs. 6.5% of White people; despite ACA-era gains, gaps persist—especially in nonexpansion states where eligibility and affordability barriers remain high. Affordability pressure is rising: only 51% of Americans can access and afford quality care, with Black adults more likely to be “cost desperate,” unable to pay for needed care or medicines. These access constraints have downstream effects on preventive services and continuity of care. [kff.org], [aspe.hhs.gov] [ons.org]
2) Quality of Care and Patient Safety
Disparities are not just about coverage; they’re about care quality once inside the system. Federal assessments show Black patients receive worse care on more than half of measured indicators, with pronounced gaps in heart disease, cancer, stroke, maternal health, pain management, and surgical care—reflecting both structural factors (care deserts, facility resources) and interpersonal discrimination/microaggressions during clinical encounters. [nationalac…demies.org], [content.naic.org]. Black patients have a story that they either experienced primarily or secondarily that shapes the level of skepticism they have with healthcare and what care they are willing or unwilling to receive.
3) Health Status and Life Expectancy
The life expectancy gap remains wide. Black Americans’ life expectancy is ~74.0 years vs. 78.4 years nationally with Black men specifically disproportionately impacted by the cumulative effects of societal stress. Self-rated health is poorer, with higher reports of fair/poor health—patterns that persisted through the pandemic recovery. [theglobals…istics.com]
Infant mortality is nearly double the national average (10.93 vs. 5.6 per 1,000 live births), signaling cumulative social and clinical inequities even before and just after birth. [cdc.gov]
4) Maternal Health: A Stark and Urgent Divide
In 2023, Black women died from pregnancy-related causes at 50.3 per 100,000 births, versus 14.5 for White, 12.4 for Hispanic, and 10.7 for Asian women—nearly 3.5× higher than White women. While the overall maternal mortality rate fell below pandemic peaks, the racial gap widened—underscoring systemic failures in access, bias recognition, and timely intervention. Notably, over 80% of pregnancy-related deaths are preventable. Recently publicized stories of Black mothers denied or delayed care highlight how interpersonal dismissal compounds risk in critical moments. [cdc.gov], [pbs.org], [sfgate.com], [detroitnews.com]. Stay tuned as we dig deeper into maternal health in the coming weeks of Black History Month.
5) Chronic Disease Burden
Black adults shoulder disproportionate burdens of hypertension (56.8% men; 61.0% women), obesity (55.9% women; 38.7% men), and diabetes—24% higher likelihood of diagnosis than the general population. These conditions multiply risk for cardiovascular events, cancer progression, pregnancy complications, and COVID-related morbidity. [cdc.gov], [theglobals…istics.com]
6) Cancer and HIV Outcomes
Across many cancer types, Black patients exhibit lower survival—even after accounting for stage and income—due to later diagnoses, care quality differences, and structural barriers to guideline-concordant treatment. National data show higher cancer death rates and consistently lower 5-year survival relative to White patients; importantly, survival gaps shrink when care processes are redesigned to ensure equitable, guideline-based therapy and barrier removal (transportation, navigation, cost support). Black people account for 43% of HIV deaths among those diagnosed and are less likely to be linked to, retained in, and suppressed by treatment—a treatment access and continuity problem more than a biology problem. [kff.org] [cdc.gov]
7) Mistrust and Lived Experience
Jennifer works as a therapist (clinical assessor/clinician) during the day, and also serves as a professor teaching in social work programs. Specifically, she teaches full-time in the evening at Chicago State University in their social work master’s program and works as an adjunct professor for an MSW program in Aurora, IL.
The core issue Jennifer identifies based on her experience working with patients is that Black and Brown communities routinely feel dismissed, mistrusted, and unseen in healthcare settings. She describes this experience as leaving patients feeling “shame, disappointed, feeling unseen”
Concrete examples of this bias showing up in their care include:
- Pain minimization: Patients’ physical and mental health symptoms are downplayed or dismissed
- Eating disorder oversight: Symptoms in Black and Brown patients are overlooked
- Communication patterns: Clinicians direct questions to companions instead of directly to patients
- Systemic resource withdrawal: Underserved neighborhoods lose access to healthcare resources, creating access gaps
History and contemporary encounters matter. A majority of Black adults (55%) report at least one negative interaction with providers (e.g., pain dismissed), and 51% believe the health care system was designed to hold Black people back. These perceptions are rooted in both historical abuses and ongoing clinical bias, and they shape care seeking strategies, including reliance on trusted community institutions and home based self management with OTC products and culturally trusted brands. [pewresearch.org], [pewresearch.org]
To overcome this bias, Jennifer employs multiple advocacy strategies:
- Patient empowerment: Educating and role-playing with patients to help them learn how to advocate for themselves in medical visits.
- Direct intervention: Accompanying patients and challenging clinicians when necessary.
- Policy work: Writing letters and supporting bills to address systemic barriers.
The Biology of Stress: “Weathering,” Allostatic Load, and Why Timing Matters
Crucially, disparities are not explained solely by personal choices or income. Evidence shows Black/White mortality gaps remain even at similar socioeconomic levels, and in some cancers Black patients with higher SES can fare worse than White patients with lower SES—pointing to structural racism across housing, employment, education, and health financing; unequal care quality; facility technology gaps; and higher outofpocket burdens for new therapies and postpartum supports. [kff.org], [centerforh…nalism.org]
The weathering hypothesis explains how prolonged, cumulative exposure to social and economic adversity and racism accelerates biological aging and deteriorates health—well before midlife. It’s supported by multiple physiological markers: [jstor.org], [longevity….anford.edu]
- Telomere shortening (a biomarker of cellular aging): longitudinal studies show that greater exposure to racial discrimination is linked to faster telomere attrition among African Americans, consistent with accelerated aging. [donaldhtay…dpress.com], [ocm.auburn.edu], [nia.nih.gov]
- Allostatic load (the multisystem “wear and tear” from chronic stress): Black adults show higher allostatic load scores across age groups, even after accounting for poverty—connecting stress biology to disparities in chronic disease risk. [longevity….anford.edu], [link.springer.com]
- Epigenetics (stress-related changes in gene expression): emerging human evidence demonstrates heritable epigenetic signatures of traumatic exposure, and studies of Black women show epigenetic aging acceleration associated with interpersonal racism. [news.yale.edu], [sph.umich.edu]
- Inflammation (elevated cytokines and oxidative stress): reviews link structural inequality and chronic stress to persistent inflammation, which drives cardiometabolic and cancer risk. [mdpi.com]
Why this matters for brands and care: Weathering shifts risk earlier in life; it also shapes how, when, and where people seek care, and how much selfmanagement happens at home. Products and messaging that assume “average” aging or risk timing can miss Black consumers’ realities and needs.
C+R POV: What Brands—Especially in CPG—Can Do Next
Bringing It Together
Black/African American consumers evaluate healthcare systems and brands through lived experience: a biological reality of weathering, a historic record of exclusion and exploitation, and a presentday landscape of affordability, quality, and respect. When brands design for earlier risk, cocreate with trusted community actors, and make equity a measurable outcome, consumers feel seen, outcomes improve, and trust grows.
1) Design for home “care work” under stress biology.
Weathering shifts risk earlier and increases self-management. Offer clear, culturally relevant guidance and bundled tools (e.g., BP cuffs with large-print tips and escalation cues; prenatal/postpartum OTC kits with red-flag checklists and QR help) grounded in clinical thresholds and when-to-seek-care triggers. [sfgate.com], [healthhistory | PowerPoint]
2) Build trust through representation + community partnerships.
Co-create with Black clinicians, doulas, and CHCs; sponsor church and HBCU-anchored activations with closed-loop navigation (transport vouchers, warm handoffs to clinics). The doula expansion model shows improved outcomes when trusted advocates are accessible. [nachc.org], [beckershos…review.com]
Jennifer emphasizes that community health initiatives must be thoughtfully designed. She recommends leveraging trusted institutions like churches for outreach, but stresses the critical importance of pairing screening with concrete follow-up—case management, transportation support, and one-stop clinics. As she puts it, “if you’re going to do it, you got to have a plan” for aftercare.
3) Reduce financial friction at critical windows.
Operationalize affordability relief—subscriptions, coupons, and sliding-scale bundles in ZIP codes with higher uninsured rates; time offers around postpartum months 0–12 when risk is elevated. Addressing cost gaps aligns with current evidence on delayed care and cost desperation. [aspe.hhs.gov], [pewresearch.org]
4) Elevate navigation and literacy with “weathering-aware” content.
Use plain-language, QR-enabled guides for chest pain, postpartum bleeding, infant fever, and BP thresholds; push SMS nudges tied to preventive care milestones. Earlier risk means earlier decision support—not just information. [sfgate.com]
5) Make equity a KPI—track and close use/adherence gaps.
Measure reach, engagement, and adherence by ZIP/community; localize retail assortment and stock reliability in maternity care deserts. Survival gaps shrink when care processes and barrier removal are deliberately designed. [ncpedia.org], [en.wikipedia.org]
6) Be precise and ethical about consent and data.
If content references Henrietta Lacks or Tuskegee, pair storytelling with how your brand handles consent, privacy, and benefit-sharing, including community advisory and data use transparency. [hopkinsmedicine.org], [grants.nih.gov], [cdc.gov]
7) Support quality and technology upgrades in underserved settings.
Where relevant (healthtech, diagnostics), fund equipment upgrades and quality-improvement pilots that document earlier stage at diagnosis and treatment completion—publishing outcomes locally. Uneven technology access deepens disparities. [nationalac…demies.org]

